Haiti is a French-speaking country located in the Americas. Apart from being close to Canada, the French Language contributed to the two countries developing a tight bond over the years.

Check out our detailed guide on what you should know about Haiti international relations with Canada, including the history and current situation.
Haiti-Canada Relations – Facts and Figures
When Was Haiti Discovered?
History tells us that China and India probably knew about Haiti for a long time before Europeans. It was Christopher Columbus who first came to the island from Europe in 1492. Columbus even established the first European settlement in the Americas on Haiti. Its name was La Navidad.
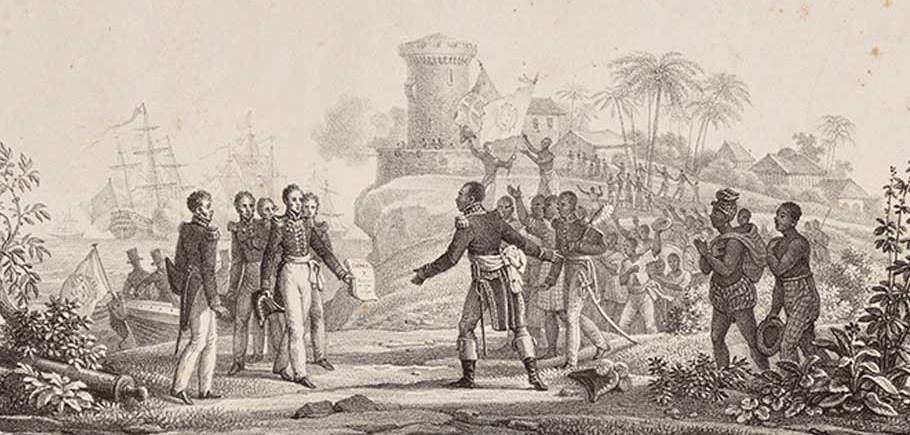
Spain claimed rights to the island, but France got involved soon. It was in 1804 when the Haitian Revolution led to independence from France. Although they still speak French, the country had become the first Caribbean independent nation in the 18th century.
Today, Haiti has a population of 11.1 million.
What Made Two Countries Cooperate?
You could say that language was what contributed the most to building Haiti Canada relations. These two countries are the only ones from the Americas, where French is the customary language. Additionally, you will find many Canadian residents of Haitian origin, which is another reason to nurture good relationships.
Canadian and Haitian People

You will find Canadian residents of Haitian descent throughout the country. They are mostly present in Quebec due to the French language spoken there. It is safe to say that the people of these two countries are getting along well. The migration from Haiti to Canada is still present, and many Haitians are leaving the island to look for a better life.
What Are the Diplomatic Relations Between Canada and Haiti Now?
We could describe the current situation in Haiti Canada relations as stable. The visit from the Prime Minister of Canada at the time, Stephen Harper (twitter), showed that the relationship between the two parties is on the right path.

International Intervention Within Countries
Two major international interventions occurred in Haiti in the last several decades. The efforts focused on assisting in delivering peace to the country dealing with political turmoil. From 1957 to 1986, the Duvalier family implemented dictatorship over the island of Haiti. That led to migration and an increased number of Haitians in Canada.

Following the overthrow of the dictatorship, Canada didn’t want to recognize the 1988 elections in Haiti since over 30 people died during the electoral process. They even cut development aid and joined an international intervention in 1993.
International Peace Efforts
Following a political crisis, the United Nations organized a mission in Haiti from 1993 to 1997. Canada provided police commissioners, and General Robin Gagnon led the Transition Mission in 1997.

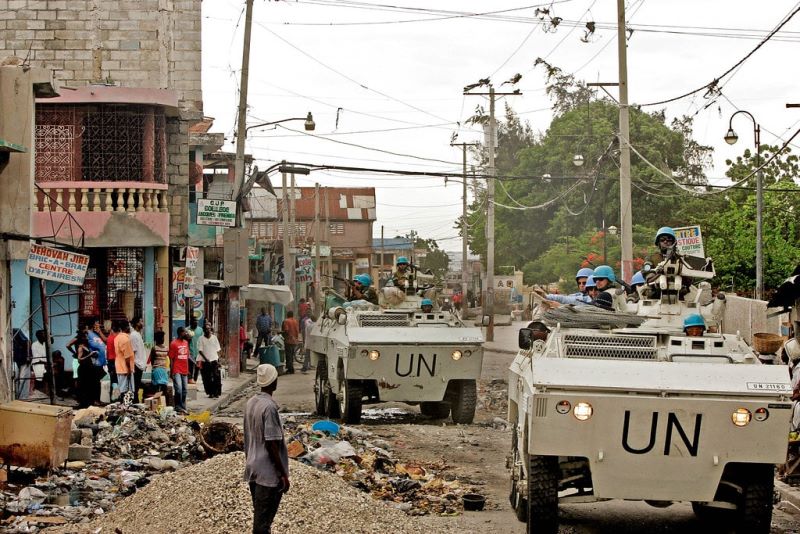

Haiti international relations with Canada were under a new test in 2004. A rebellion overthrew the current president, and the UN sent another stabilization mission. From then, it seems that the situation on the island has been far more stable.
The Canadian Armed Forces in Haiti
Haiti’s political situation was in chaos during the 1990s. The Haitians in Canada urged the country to intervene, which they finally did in 1993. According to the estimates, 500 members of the Canadian Armed Forces were sent to Haiti to help establish peace. That included transportation, engineering, aviation, and other personnel.

The same thing happened during another crisis in 2004, where Canada played a role of maintaining peace until the United Nations arrive.
Countries’ Membership in International Organizations

Haiti and Canada are both members of La Francophonie. It is a worldwide organization gathering countries where French is customary or bridge language, and a considerable proportion of people speak this language.
Canada and Haiti are the only two members from the Americas, but the organization gathers more than 80 countries. These two countries are also members of the OAS – Organization of American States and the United Nations.
Canadian Embassy in Haiti
Canadian Embassy in Haiti is in Port-au-Prince, which is the capital of the country. Once the Canadians established official diplomatic relations with Haiti in 1954, it was Edward Ritchie Bellemare, who was first at the helm of this embassy.

Today, the Canadian embassy work on getting two countries closer and help citizens with various traveling and administrative services.
The World Responds to Haiti-Canada Diplomacy
Whenever Canada asked for help for Haiti international relations, they received it. The country helped this island on numerous occasions, including food programs, development aids, etc. Canada was among the leading countries that helped Haiti after the devastating earthquake in 2010. They gathered over $400 million and rallied other parts of the world to help. The world responded to this diplomacy, and Haiti received significant aid in dealing with the consequences of the earthquake.
Mission to Haiti Canada

Mission to Haiti Canada is a charitable organization established in 1997. Volunteers lead this organization whose mission is to empower the people of Haiti with skills and other resources required to improve their quality of life. You can get involved with the program as both a volunteer and a sponsor. Whether you want to go on a mission trip, collect medical and other items, or provide financial support, you are welcome.
Stay Updated: Exploring the Ever-Evolving Haiti-Canada Landscape
Haiti and Canada share a brief but intricate history of international relations. From the Haiti Network, YouTube videos capturing the Haiti elections in action, to the quaint coastal town of St. Marc in Haiti, there is always something newsworthy happening between these two nations. If you’re looking for the latest updates on Haiti, St. Marc is a place to keep an eye on. With its vibrant culture and bustling streets, it often finds itself at the center of Haiti’s last news. Haiti Liberte, a prominent news source, covers the latest developments in Haiti, ensuring that readers are up to date with the country’s ever-changing landscape. From news articles on Haiti to the most recent happenings, there is no shortage of information available. Notably, housing remains a pressing concern in Haiti, and the latest news sheds light on the ongoing efforts to address this issue. With cash work initiatives and aid to Haiti, progress is being made, and the latest updates reflect this positive trend. So, whether you’re interested in the latest Haiti news, the recent developments in aid, or the ever-evolving landscape of Haiti’s international relations, staying informed will help you navigate this dynamic and resilient nation.
